New Medical Director of Emerging Infectious Diseases Faces First Test, Succeeds in Monkeypox Outbreak Response
Marc Couturier, PhD, has always understood the potentially devastating consequences of an infection, whether it’s an isolated case or a pandemic that affects millions.

Marc Couturier, PhD, has always understood the potentially devastating consequences of an infection, whether it’s an isolated case or a pandemic that affects millions.
In college, Couturier watched two of his friends experience protracted battles with chronic infections of Helicobacter pylori, bacteria that infects the stomach.
“I saw how much they struggled with their diagnosis and treatment, and I remember thinking that two 20-year-old, healthy young men shouldn’t be that miserable. There’s got to be something we can do—something we can understand better or get better at diagnosing and treating,” Couturier said.
One of Couturier’s friends made a full recovery; the other developed multiple complications that led to an even more prolonged course of treatment.
That college experience sparked Couturier’s lifelong dedication to better understanding infections and improving diagnostic methods and fed his keen interest in helping communities respond to outbreaks.
When leaders at ARUP Laboratories realized they needed an individual who would be responsible for responding to emerging infectious diseases, Couturier was a natural choice for the role.
“I made the decision to create a medical directorship for emerging public health crises so that going forward, we would have somebody who would track the progress of these infections and could direct Research and Development on which assays to develop, knowing that not everything becomes a public health epidemic,” said Tracy George, MD, ARUP president and chief scientific officer. The new role grew out of the experience ARUP gained in bringing a new test online quickly and scaling up capacity rapidly during the COVID-19 pandemic.
Couturier became medical director of Emerging Public Health Crises in January 2022. Five months later, he faced his first test when monkeypox cases in the United States began to rise. Couturier tracked the progress of the outbreak and coordinated with his contacts in public health to ensure that ARUP responded efficiently and appropriately to the emerging disease.
In this new position, Couturier was able to raise the alarm on the developing monkeypox crisis and bring ARUP teams together to respond quickly to the public health emergency. ARUP’s success in providing a testing solution with the capacity to support the needs of communities across the U.S. demonstrated the effectiveness of Couturier’s new role.
“Marc was perfect for this role, given his medical expertise in infectious diseases as well as his innate curiosity, his enthusiasm for issues concerning public health, and his skill at building relationships that are key to success when these outbreaks occur,” said Jonathan Genzen, MD, PhD, ARUP chief medical officer.
Expertise and Experience in Multiple Outbreaks
After receiving his doctorate degree in medical microbiology and immunology with specialization in bacteriology from the University of Alberta in Canada, Couturier worked as a postdoctoral fellow at the Alberta Provincial Laboratory for Public Health.
“That was my first introduction to pandemic response and seeing a laboratory develop a test quickly,” he said. “I was exposed to many other pandemic response processes, infrastructure, and systems that were in place in the Canadian public health system.”
Couturier was working at the Alberta laboratory during the first early wave of the 2009 H1N1 pandemic, where he experienced an outbreak from the perspective of both laboratory expert and patient. While he was participating in conversations with public and government officials on how to proceed with social mitigation efforts, his wife was expecting their first child. They spent time in the hospital, where they saw firsthand the segregated, makeshift hallways where those who had flu-like symptoms could be kept separate from other patients and visitors.
Shortly after his experience in Alberta, Couturier relocated to Utah to continue his work in infectious diseases. He completed a fellowship in medical microbiology at the University of Utah School of Medicine, where he now serves as a professor in the Department of Pathology. He is also the medical director of Parasitology/Fecal Testing and Infectious Disease Antigen Testing at ARUP Laboratories.
“My recommendations in handling monkeypox have been informed by my experiences at ARUP for the past 11 to 12 years, including our experiences with the Zika virus and COVID-19,” Couturier said. “Since I entered the field, I’ve been involved with 10 different epidemics or pandemics of some kind that have required an immediate or urgent response from the laboratory.”
Launching a State-of-the-Art Assay for Monkeypox Infections
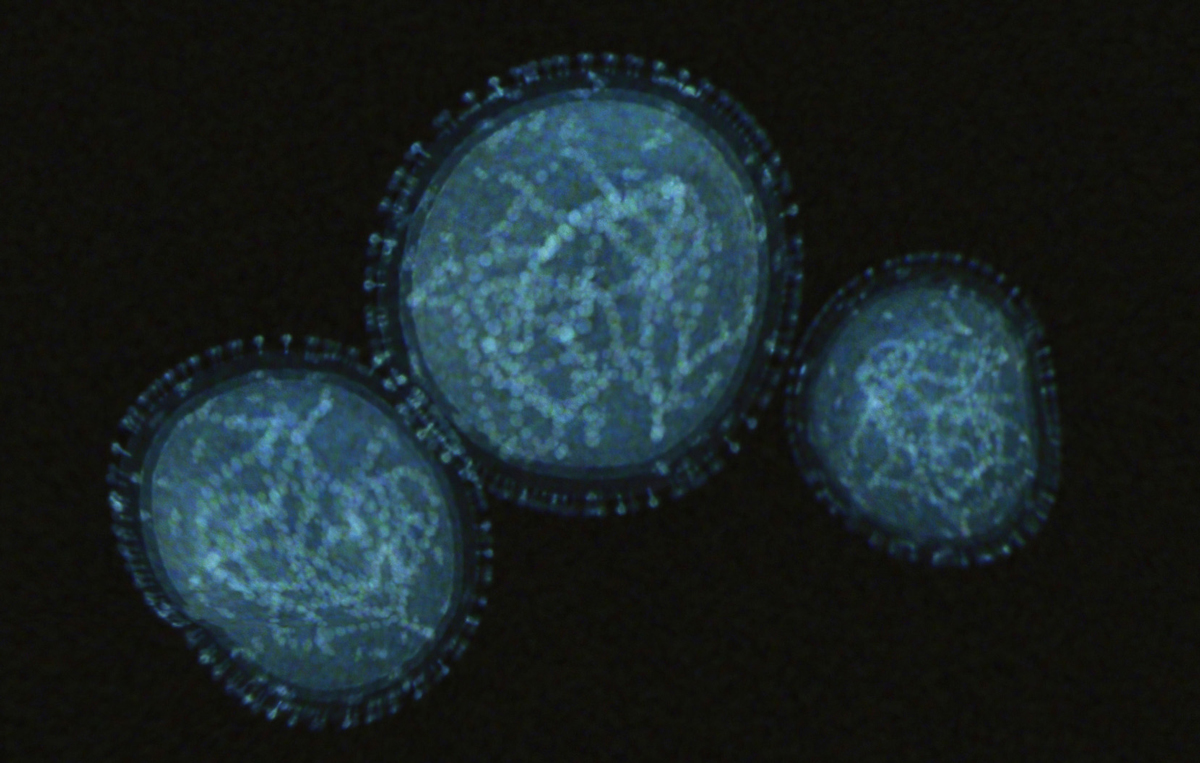
As a result of Couturier’s attentiveness and the efforts of many others, ARUP launched its test, Orthopoxvirus (includes monkeypox virus) by PCR, on July 25, 2022, within just a few weeks of initiating development. ARUP was also one of the first labs to implement a test that was designed for more modern processes and automated testing platforms.
“ARUP developed a state-of-the-art, automated test that has great turnaround times, is scalable to meet capacity, and meets the needs of patients in the United States,” George said.
Experts at ARUP chose to design their own, modified assay rather than use the current CDC assay, which was designed in 2005. The CDC’s assay was validated for dry lesion swabs that require a manual, labor-intensive extraction method that slows down the entire testing process and takes much longer to yield results. ARUP’s test was instead validated for use with swabs in viral transport media (VTM), which can be processed without requiring a manual extraction process.
“It would have been disruptive to attempt to incorporate the CDC’s test as it was into our existing workflows,” Couturier said. “While it was difficult to turn away an assay that was already packaged, we chose to develop a test based on the CDC’s assay but optimized to fit in the systems we already had in place. Because of that decision, we were able to support higher volumes right out of the gate.”
That higher capacity proved invaluable once specimens began to arrive at ARUP for testing. Although there was not the dramatic explosion in test demand that the world witnessed during the COVID-19 pandemic, the testing volumes for monkeypox rose quickly, expanding from just a handful of tests per day to hundreds.
After the launch of its first test, ARUP immediately began working to validate an even higher-throughput testing platform, the Roche cobas 6800, that further increased ARUP’s testing capacity.

“We quickly realized that we needed to develop a second assay because of all the supply chain issues that ARUP dealt with during COVID-19,” George said. “The transition from validation in Research and Development to production in the laboratory went smoothly because each person understood their role.”
ARUP launched the second version of its orthopoxvirus assay within three weeks of initiating the validation, completing an extensive process that normally takes several months.
“We’ve done a much better job of identifying key stakeholders—everyone from medical directors to lab to Purchasing to Safety to Communications teams. Everyone is in this, and there are no silos. This allows separate processes to move forward concurrently, creating significant efficiency in how quickly we can complete the necessary tasks,” Couturier said.
Implementing a Comprehensive Pandemic Response Plan
Appointing Couturier to his new role is just one aspect of ARUP’s new comprehensive pandemic response plan.
“We didn’t have anyone at ARUP who was specifically tasked with monitoring emerging infections. We needed to identify an expert in the field who could not only pay attention to emerging diseases, but who could advise ARUP’s executive emergency response team about when to enact the pandemic response plan, and about the right level of response and timing,” said Margaret Coppin, HT(ASCP), ARUP quality officer.
After COVID-19, ARUP leaders moved to capture the lessons learned during the pandemic to ensure ARUP could respond quickly and effectively to new infections.
Coppin and her team of quality professionals evaluated the events that occurred during COVID-19 to formulate a comprehensive pandemic response plan that is based on the same quality standards that form the foundation of all testing at ARUP.
“We already had a very robust disaster response plan, but there were some nuances with bringing a test online quickly that we learned from COVID-19,” Coppin said. “The pandemic response plan acts as a checklist to ensure that everyone understands who is ultimately responsible for completion of certain tasks and to prevent team members from working at cross-purposes.”
The pandemic response plan also provides a pathway for ARUP experts to complete the necessary steps that ensure the test operates as expected and to the highest quality standards.
“The quality systems essentially form the framework of our pandemic response plan and illustrate our focus on quality. The plan incorporates the quality indicators, metrics, and quality assurance checks that we build into any other test to ensure that we can carry out a rapid response to meet patient needs while also ensuring that we are not compromising on quality,” Coppin said.
Now that the pandemic response plan has proven effective and helpful, Coppin and her team will investigate ways they can implement elements of the new plan into the existing emergency response plan as part of their commitment to continually improve ARUP’s preparedness for unexpected events.
Collaboration Between ARUP and Other Labs Improves Community Outcomes

In addition to the new pandemic response plan, increased collaboration between ARUP and other laboratories has improved overall accessibility to testing during the monkeypox outbreak.
ARUP has worked closely with the Utah Public Health Laboratory. Its current Clinical Laboratory Improvement Amendments (CLIA) laboratory director, Alessandro Rossi, PhD, D(ABMM), is a former ARUP fellow.
“The Utah Public Health Lab was absolutely integral to ARUP’s effort to develop a monkeypox assay. They were able to share known positive and known negative samples that they had tested early in the outbreak that enabled us to validate our assay,” Couturier said.
In return, when the Utah public lab needed samples to validate another specimen type for its assay, ARUP was able to provide those samples.
“Marc has previous training in public health, so he understands the mindset and culture to work with us as a state lab. Marc realizes the importance of working closely with public health to help the entire community,” Rossi said.
Rossi was a fellow at ARUP from 2015 to 2017 and continues to collaborate with ARUP on several research studies, in addition to working with ARUP on the COVID-19 and monkeypox outbreaks.
“The government has been more proactive in involving private laboratories in responding to this new pandemic threat to quickly build capacity. The CDC has shared protocols for reference labs such as ARUP to bring on a test for monkeypox infections,” Rossi said.
At the time the CDC released protocols for monkeypox testing, the state labs were operating only at an average of 10% capacity. However, while many labs were well under capacity, some state laboratories were beyond 100% capacity in particularly heavy-hit areas. To prevent the state laboratories from becoming completely overwhelmed, the CDC moved much more quickly to involve private laboratories, in contrast to the delayed response during the COVID-19 pandemic.
In addition to sharing specimens for validation, the Utah public lab also meets monthly with clinical partners in the state, including ARUP and Intermountain Healthcare, to discuss emerging infections and the best approaches to minimize their impact on Utah communities. This type of collaboration is something that may not have been common before COVID-19 and is one silver lining to emerge from the pandemic.
“Having a good relationship with a reference or private lab means it can absorb capacity when the state lab becomes overwhelmed. This has not yet happened for monkeypox, but the state relied on ARUP several times during COVID-19, and ARUP has always been there for us,” Rossi said.
Enthusiasm for Community, Innovation Beyond Infectious Disease
Since his college friends’ battles, Couturier has become an expert in H. pylori infections, pushing the boundaries to understand its pathogenesis and antibiotic resistance and methods to diagnose it, and has investigated its prevalence in communities in Utah.
Couturier has also advanced the use of artificial intelligence (AI) solutions at ARUP, leading the development of the world’s first AI-augmented ova and parasite assay. The AI-augmented tool uses a convolutional neural network to identify ova and parasites in scanned images of stool samples.
“He’s a firm believer in pursuing the leading edge of new technologies and applications that will improve our testing and decrease turnaround time. Not only is he extraordinary in his technical expertise, but he has a public mindset and is intent on contributing to the health and welfare of people,” said Lisa Skodack-Jones, an ARUP clinical product manager in areas of infectious disease and immunology who has continued as a consultant for ARUP after her retirement in late 2021.
Couturier’s community initiatives extend outside the realm of infectious diseases. He has also been heavily involved in helping build the hockey community in Salt Lake City, and he coaches the local teams of both his son and daughter.
“His heritage is French Canadian, so that’s where the hockey comes from,” Skodack-Jones added.
“This new position has been an absolute pleasure. It has allowed me to liaison with so many different groups within ARUP and others at the local and national levels,” Couturier said. “Seeing all these groups and individuals work cohesively toward the betterment of public and community health during times of need is a fundamental example of what brought me into this field from the beginning.”